How “Critical Incidents” Can Happen in Rehab Care
A critical incident is a serious event that needs fast action. In a rehab setting, it can include:
- A medical emergency like trouble breathing, seizures, or fainting
- A suspected overdose and a need for rapid emergency management
- A serious adverse event during treatment, like a dangerous medication reaction
- A safety threat, like violence, self-harm risk, or leaving the program unexpectedly
During these moments, the goal is simple: protect the patient, support the care team, and lower risk.
Why Labs Matter During a Critical Incident
A rehab center can do many things on-site. But a trusted laboratory partner helps with one big need: clear, reliable diagnostics.
A lab like Lynk Diagnostics supports rehab centers by:
- Confirming drug testing results with strong clinical methods
- Helping staff understand what results may mean (and what they do not mean)
- Supporting proper documentation for safety, quality, and management reviews
- Offering dependable customer service so staff can get answers quickly
Labs do not replace medical care. But they can be a key tool during urgent decision-making—especially when the care team must act fast and stay fair.
Collaboration Starts Before Anything Goes Wrong
The best collaboration happens before a crisis.
Rehab centers and Lynk Diagnostics can align on:
- Shared goals for patient safety and quality care
- Clear policies for “what to do next” when results are unexpected
- Staff education on sample collection, privacy, and documentation
- Communication steps: who calls who, and how fast
When an organization plans ahead, a critical incident is still hard—but it becomes more controlled and less chaotic.
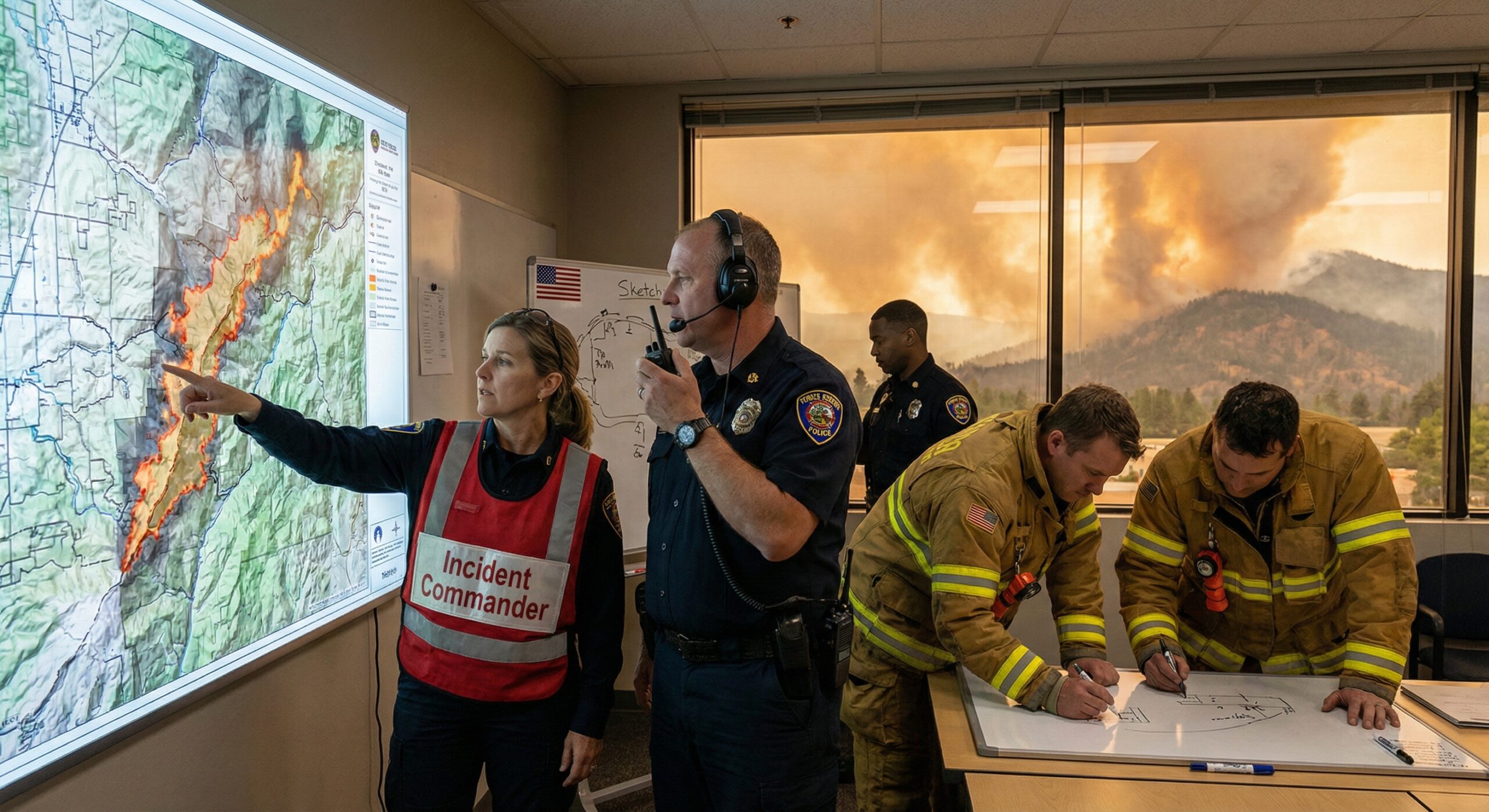
What Happens First During an Emergency
When a true medical emergency happens, the priority is always the person’s life and health:
- Staff follow the facility’s emergency plan
- They may call 911 and involve the emergency department
- A physician (or medical provider) may guide next steps
- The team documents the incident in the record
If opioid overdose is suspected, naloxone may be used if staff are trained and allowed under local rules and protocols. (Naloxone can reverse opioid overdose when given in time.)
How Drug Testing Fits Into Critical Incident Response
Drug testing is not “gotcha” medicine. In rehab care, it is used to support safety and treatment planning.
During a critical incident, drug testing may help the team:
- Understand possible exposure that affects breathing, heart rate, or behavior
- Check if relapse may be connected to the event
- Support safe medication decisions
- Reduce confusion and help the care plan stay focused
That said, drug test results must be handled carefully. Some tests are screening tests, and some are confirmatory tests. The lab helps explain that difference so decisions are based on strong evidence—not assumptions.
The Lab’s Role: Fast, Clear, and Clinical Support
During critical incidents, Lynk Diagnostics focuses on:
- Communication that is quick and respectful
- Clear explanations in plain language
- Clinical support for interpreting results (within appropriate scope)
- Proper handling and documentation as a reference lab partner when needed
The lab also helps the rehab center avoid common mistakes, like:
- Treating a screening test as a final answer
- Forgetting to consider prescriptions or treatment medications
- Missing steps that protect sample integrity and reporting accuracy
Using Data the Right Way
In a crisis, data can help—but only when it is organized and accurate.
Labs and rehab centers often use:
- Secure reporting portals and lab result delivery systems
- Technology that supports fast access to results
- Practice rules for who can view results and when
When possible, results may be connected to the electronic health record (EHR). This helps the care team document what happened, what was done, and what the plan is next. It also supports continuity if the patient is transferred to a hospital or higher level of care.
Software, Privacy, and “Need-to-Know” Access
Critical incidents bring stress, and stress can lead to oversharing. That’s why strong privacy practices matter.
A good system uses:
- Secure software and encrypted systems
- Role-based access (only staff who need it can see it)
- Clear rules for sharing results with outside providers
This protects health information and supports trust—inside the rehab center and across the community.
“Shared” Communication: How Teams Stay on the Same Page
During a critical incident, confusion is dangerous. So collaboration needs structure.
A strong “shared plan” includes:
- One point of contact at the rehab center (often nursing leadership or management)
- One point of contact at the lab (client support/customer service)
- A clear call path for urgent questions
- A shared timeline (what happened first, next, and last)
This kind of collaborative approach supports safer decisions and better teamwork between rehab staff and labs.
Supporting Learning After the Incident
After the emergency ends, the work is not over. Now it is time for learning and improvement.
Many health care groups use structured reviews after serious events. For example, The Joint Commission’s Sentinel Event policy emphasizes careful investigation and corrective action after serious patient safety events.
Rehab centers may do a review like:
- What happened?
- What were the safety gaps?
- What can we change so it doesn’t happen again?
A lab can support this learning by:
- Providing test timelines and reporting details
- Explaining what the results can and cannot show
- Helping update workflows, training, and documentation
Critical Incident Examples Where Lab Collaboration Helps
Here are a few real-world style examples (not patient-identifying):
Unexpected behavior change and safety risk
A patient becomes confused and unsafe. The team worries about relapse, medication interactions, or a medical issue. Lab results may help guide the next clinical steps while the care team monitors safety.
Possible overdose and emergency transfer
A patient has signs of overdose. Emergency response begins. Later, lab results and clinical notes help the rehab team coordinate return-to-care planning and safer treatment supports. CDC explains naloxone is a life-saving medicine that can reverse opioid overdose when given in time.
Medication questions during treatment
A provider needs to know whether a result could be from a prescribed medication. The lab can help explain testing methods and confirmatory steps so care is accurate and fair.
How This Collaboration Protects the Whole Organization
Critical incidents can affect:
- The patient’s health and recovery path
- Staff stress and confidence
- The rehab center’s reputation and regulatory standing
- Documentation and reporting requirements
Emergency planning is also a major expectation across health care settings. CMS outlines emergency preparedness expectations for Medicare/Medicaid participating providers and suppliers.
When labs and rehab centers work together, it supports:
- Stronger safety culture
- Better documentation
- Clearer decisions during high-pressure moments
- Lower long-term risk
Choosing the Right Lab Partner for Critical Incident Support
Not all labs support rehab care the same way. A lab partner should bring:
- Reliable testing methods and quality controls
- Fast turnaround pathways when clinically appropriate
- Clear escalation paths during urgent situations
- Strong customer service and communication
- Respect for the patient and the treatment process
At Lynk Diagnostics, the focus is on supporting rehab centers with consistent processes, clear reporting, and collaboration that keeps patient safety first.
FAQs
What is a “critical incident” in a rehab center?
A critical incident is a serious event that needs fast action to protect safety, like a medical emergency, overdose risk, severe behavior crisis, or another major adverse event.
How can a lab help during a critical incident?
A lab can provide reliable diagnostics, explain results clearly, and support documentation and communication—so the treatment team can make safer decisions.
Do drug test results prove what caused an emergency?
Not always. A result is one piece of data. Clinical signs, provider evaluation, and the full health picture matter too. The lab helps explain what results mean and what they don’t mean.
Why does the electronic health record matter during emergencies?
The electronic health record helps keep information organized. It supports clear documentation, safe handoffs, and better communication if the patient needs emergency department care.
What happens after the incident is over?
Many centers do a review to learn what happened and reduce risk going forward. This can include policy updates, education, and workflow changes with shared goals for safety.